
Approximately half of infections occur within 2 weeks of surgery, but delayed infection do occur up to a year after surgery. Infectious keratitis: There is a risk of corneal infection after RK.Its 10-year data was published as the PERK (Prospective Evaluation of Radial Keratotomy) study, which proved the onset of progressive hyperopia – often found a decade after the original surgery – is due to continued flattening of the central cornea. Progressive hyperopia: RK enjoyed great popularity during the 1980s, and was one of the most studied refractive surgical procedures.
In cases where large epithelial plugs lead to such aggravating symptoms, patients may seek further surgical treatment to alleviate the symptoms. These dark conditions cause the pupil to dilate, maximizing the amount of scattered light that enters the eye. Visual phenomenon: Large epithelial plugs may cause more scattering of light, leading to the appearance of visual phenomena such as flares and starbursts – especially in situations such as night driving, where the stark light of car headlights abounds.Similarly, infection of these chronic wounds can also occur years after surgery, with 53% of ocular infections being late in onset.

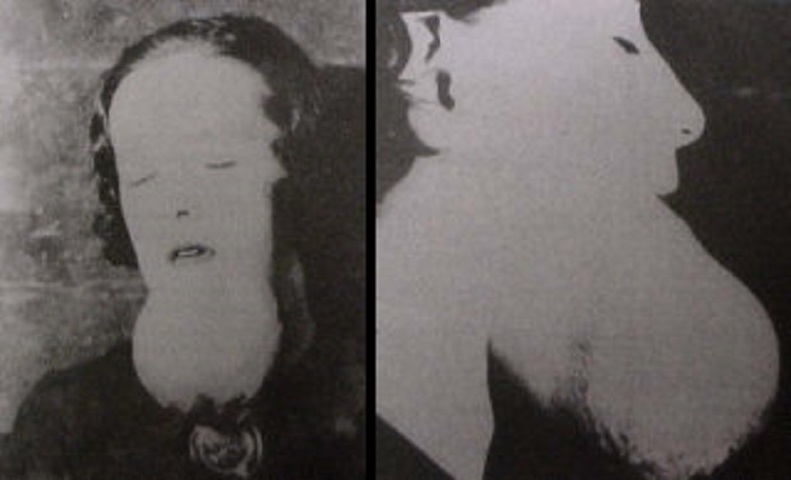
The risk is estimated to be between 0.25% and 0.7% Healing of the RK incisions is very slow and unpredictable, often incomplete even years after surgery. This, consequently, leaves the cornea more susceptible to infections. As the cells migrate from the depth of the plug up to the surface, some die before reaching it, forming breaches in the otherwise healthy epithelial layer. Often this plug is three to four times as deep as the normal corneal epithelium layer. Closer to the wound surface lies the epithelial plug, a bed of the cells that form the normal corneal epithelium which have fallen into the wound. The healing corneal wounds consist of newly abutting corneal stroma, fibroblastic cells, and irregular fibrous connective tissue. Example of a desirable outcome (left), and an undesirable outcome (right). Postsurgical healing Ĭross-section schematic of postsurgical epithelial plugs. Despite this, 70% of patients reported not requiring corrective lenses for distance vision 10 years after surgery. From 2 to 10 years post-operatively 43% of eyes had an increase in farsightedness by 1.00D or more. Additionally, 76% of eyes had uncorrected vision of 20/40 or better at 3 years. According to the PERK study, 58% of eyes were corrected within 1.00D of goal 3 years after surgery. The procedure results in a decrease in nearsightedness. Other sources cite surgeries leaving 20 to 50 micrometres of corneal tissue unincised (roughly equivalent to 90% of corneal depth, based on thickness norms). One study cites incisions made to a depth equivalent to the thinnest of four corneal-thickness measurements made near the center of the cornea. Incisions that penetrate only the superficial corneal stroma are less effective than those reaching deep into the cornea, and consequently, incisions are made quite deep. Typically, between 4 and 24 radial incisions are made in a number of patterns and orientations based on refractive errors, surgeon style and surgeon training. RK may be performed with different types, numbers, and patterns of incisions. The original technique – consisting of incisions from periphery to center – was called the "Russian technique", while the later advances of performing controlled incision from center to periphery was called the "American technique". The incisions relax the steep central cornea in patients with myopia in order to achieve a decreased need for correction. When performing RK, incisions are made with a diamond knife. It has been largely supplanted by newer, more accurate operations, such as photorefractive keratectomy, LASIK, Epi-LASIK and the phakic intraocular lens. It was developed in 1974 by Svyatoslav Fyodorov, a Russian ophthalmologist. Radial keratotomy ( RK) is a refractive surgical procedure to correct myopia (nearsightedness).


 0 kommentar(er)
0 kommentar(er)
